What affects Part B beneficiary premiums?
The Part B premium amount for a particular beneficiary may vary based on several factors, including:
- Hold Harmless Provision: guarantees the amount of the SS income payment net of Part B premiums is at least as great as the year prior (if the Part B premium is deducted directly from the enrollee’s SS payment). This provision is intended to protect beneficiaries against Part B premium increases that would exceed the SS cost-of-living adjustment (COLA). This may reduce the effective Part B premium paid by certain beneficiaries, while increasing the premium for other beneficiaries not held harmless (to target the same 25% of overall expenses).
- Income Related Monthly Adjustment Amount: requires beneficiaries with higher income to pay higher Part B premiums. This adjustment reflects a sliding scale to the Part B premium to cover 35-85% of the total Part B program costs.
- Late Enrollment Penalty: requires beneficiaries who enroll late in Medicare Part B (after 12 months of eligibility) to pay a penalty when they elect to enroll.
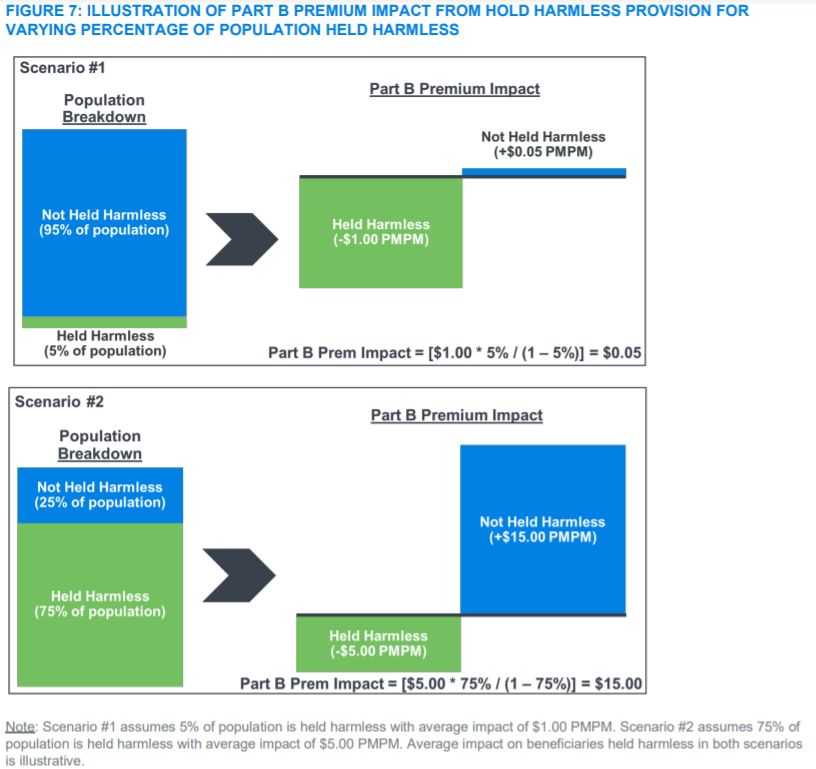
In order to maintain that 25% of the total Part B program costs are collected through premiums, there are some scenarios where the premium impact of beneficiaries held harmless could shift to beneficiaries not held harmless. This provision could have a cascading increase on the premiums for beneficiaries not held harmless.
Milliman modeled the Part B premium dynamics of the hold harmless provision for beneficiaries held harmless and those not held harmless. Figure 7 of the Milliman report includes two illustrative scenarios:
- 5% of the population is held harmless with a $1 average reduction to their premium
- 75% of the population is held harmless with a $5 average reduction to their premium
The premium impact is leveraged as when more beneficiaries are held harmless, there is a smaller population to spread the costs across.
More details on Medicare Part B program costs’ impact, stakeholder considerations, methodology, and limitations can be found here.