New Therapeutics Prove Beneficial. So Why Are People Still Dying?
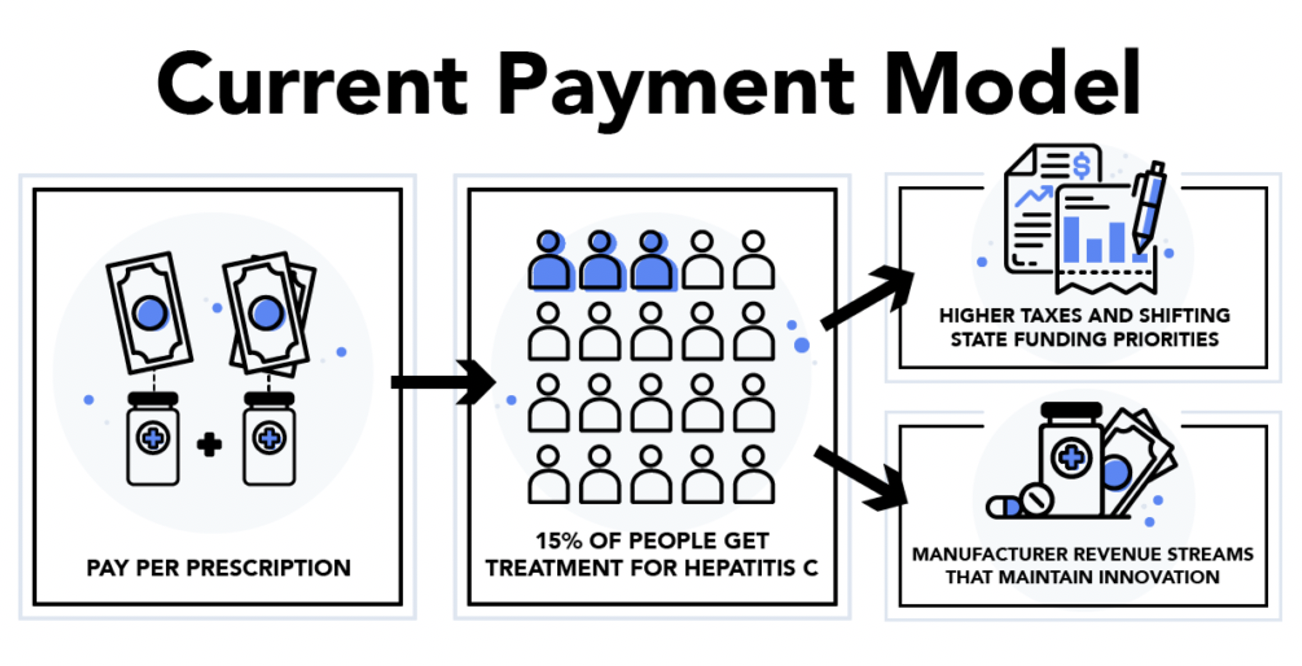
Though effective HCV treatment is available, the high drug prices prevent a majority of Hepatitis C patients from accessing life-saving, curative therapeutics. A recent estimate suggests only 15 percent of the more than 3 million HCV patients in the United States have been treated. The current per prescription model for funding treatment is insufficient to pay for its high cost.
Compounding the problem, States are often responsible for this financial burden, paying the drug costs for their HCV infected citizens in prison, on Medicaid, and recipients of city and state pensions. However, many states’ budgetary constraints limit not only the purchase of these very expensive drugs but treating these patients in the most efficient way.
As reported in their study published in the November 20, 2018 issue of the Journal of the American Medical Association, Dr. Peter Bach and colleagues explained, “the best way to treat HCV is at the population level, that is, by treating every patient possible, with as much speed as is possible. Doing so would reduce the health consequences for those infected, generate the most future savings from improved health, and help decrease future transmission of HCV from person to person.”
The best way to treat HCV is at the population level, that is, by treating every patient possible, with as much speed as is possible.
New Research Proposes a “Netflix Model” to Help States Pay for Hepatitis C
Responding to the challenge, Dr. Peter B. Bach, Director of Memorial Sloan Kettering’s Dug Pricing Lab, and co-authors Mark R. Trusheim of the Massachusetts Institute of Technology and Dr. William Cassidy, former governor of Louisiana and a United States Senator, developed a new approach to pay for the life-saving drugs for Hepatitis C at an affordable or discounted price.
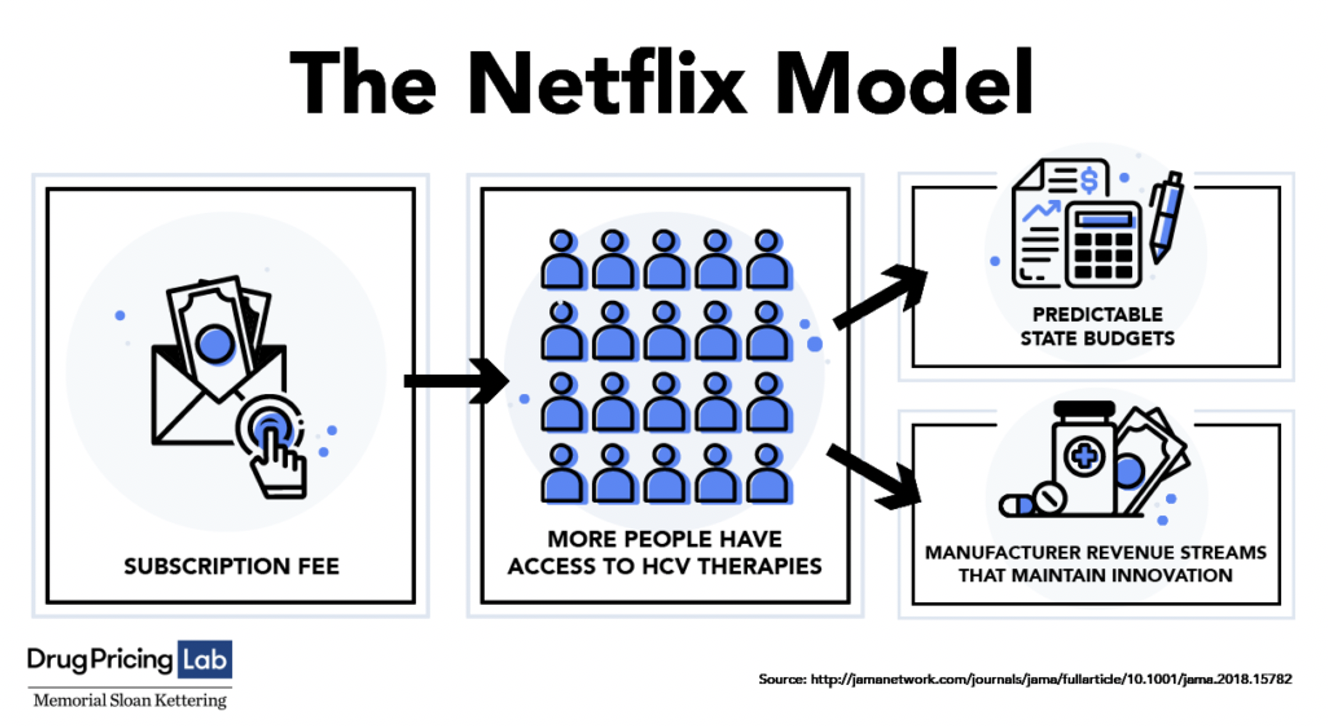
In their JAMA Viewpoint study, “Alternative State-Level Financing for Hepatitis C Treatment – The “Netflix Model,” they proposed a novel subscription-based system borrowed from popular culture and called it the “Netflix Model.” Just like a Netflix customer who pays a single fee that allows for unlimited rentals, a state government and drug manufacturers would have to agree to a lower price for unlimited Hepatitis C drugs for Medicaid patients and incarcerated persons. For the payment system to work, a state would need a buy-in from all parties involved.
Louisiana Begins A Dialogue with its Stakeholders
On August 7, 2018, the Louisiana Department of Health issued a Request for Information on the “creation of a subscription-based payment model for Hepatitis C medication”. Using the Netflix prototype, “the state would pay a drug manufacturer or manufacturers for unlimited access to this treatment for all individuals in Louisiana who are enrolled in Medicaid and in Louisiana’s correctional system. The payment to the manufacturer would be equal to or less than what the state is currently spending to provide the antiviral medication to these populations.”
The Health Department officials described their problem. “About 30,000 people in Louisiana’s Medicaid program and prison system are carrying Hepatitis C. The state cannot afford to treat large numbers of patients at current drugs prices. Because of the high cost of the drug, less than 3 percent of this population was treated in Medicaid last year. Therefore, the Department is pursuing innovative payment models which will enable the state to dramatically expand access to the drug and eventually eliminate Hepatitis C as a public health problem.”
To organize the stakeholders for the purpose of discussions, the Louisiana Department of Health utilized a broad-based steering committee which included representatives from managed care organizations, health insurers, pharmaceutical companies, health providers and municipal unions. They explored promotion, surveillance, and funding options to eliminate barriers to Hepatitis C patients receiving appropriate treatment as a first step.
Asegua Therapeutics, a subsidiary of Gilead Sciences, agreed to charge a reduced price for the Hepatitis C drug, pointing to the benefit the subscription payment model “could create predictable expenditures for the state while ensuring broad access as part of a [hepatitis C virus] elimination strategy.” The plan also presented an opportunity to align incentives to “maximize patient access to curative therapy”. Gilead explained the cost-effectiveness of this model to Medicaid and the potential for future savings to Medicare and to other payors.
Dr. Bach Explains the “Netflix Model” to US Senate Finance Committee
On January 29, 2019, Dr. Peter B. Bach, testified before the United States Senate Finance Committee in “Drug Pricing in America: A Prescription for Change, Part I”. He explained how the model (co-authored by Mark R. Trusheim and Sen. William Cassidy and originally reported in JAMA), “solves a problem specific to the Hepatitis C market”.
“There are highly effective (HCV) treatments that have prices far higher than most states can afford”, explained Dr. Bach. The drug’s cost prevents “HCV infection being essentially a one-time problem amenable to a single elimination effort that would decrease prevalence very sizably and thus reduce infection rates,” he said. A further roadblock is a “collapsing volume of sales despite price discounts” in poor states and projected to negatively affect the prospects for sales in the long run.
The co-authors proposed “a purchasing coalition within a state would run an auction to obtain a market-based price for flat subscription payments for a set number of years during which time the coalition would work with the winning manufacturer to eliminate HCV infection in the state”. Dr. Bach reported their “idea has begun to take shape in several states, with Louisiana and then Washington — posted solicitations for manufacturers to participate in a subscription-based payment model to treat HCV infected residents.”
Louisiana Agrees to 5-Year “Netflix” Hepatitis C Drug Payment Model
The Louisiana Department of Health continued to hold discussions with representative stakeholders. The health insurer United Healthcare agreed to share their research findings on the viability of a subscription payment model in Louisiana. After a clear determination of its benefits, they were able to negotiate terms to go forward with the “Netflix” financing model.
In June 26, 2019, Governor John Bel Edwards announced the launch of a hepatitis C innovative payment model with Asegua Therapeutics. “This new model has the potential to save many lives and improve the health of our citizens. It is an important day for our state, for our partner, Asegua Therapeutics, for providers, but most importantly for the patients and their families who will benefit from treatment,” said Governor Edwards.
“Asegua was willing to come to the table to work with us to help Louisiana residents and we are pleased to initiate this five-year partnership. Ultimately, our goal is to eliminate this disease in Louisiana, and we have taken a big step forward in that effort,” said the Governor.
This agreement gave Louisiana’s Medicaid patients and the state’s incarcerated population unlimited access to the Hepatitis C drug over a five-year period. Representatives of the Louisiana Department of Health said they hope to “treat at least 30,000 people by 2024.”