Copay Assistance: The Epipen Example
What happens when a patient uses a copay coupon?
A real world example of Mylan's copay coupon for Epipens to demonstrate the effects of such copay assistance programs.
With the rising costs of specialty therapies, patients are increasingly turning to copay assistance programs and copay coupons offered by manufacturers to alleviate the financial toxicity associated with the costs of their drugs. Simultaneously, pharmaceutical companies are offering more and more of these coupons- a NEJM Perspective by Dafny et al. estimated that half of noninjectable, brand-name drug revenue was derived from drugs with copayment coupons in 2010, a twofold increase since 2007.
While copay coupons superficially appear to benefit patients, they actually contribute to increasing health care costs. Dafny et al.'s team concluded that between 2007 and 2010, spending on 23 drugs with coupons was $700M to $2.7B higher than if coupons had not been utilized. The harms of such programs were also detailed in the Annals of Internal Medicine, in a piece by Drs. Peter A. Ubel and Peter B. Bach:
It might seem like a reasonable deal for everyone when pharmaceutical companies fund a portion of the price of their own medications through coupons or charitable contributions. But pharmaceutical companies do not offer assistance for all filled prescriptions, only for those that patients fill before their insurance kicks in. When patients reach their out-of-pocket maximums, insurers pay all future costs. Because insurers cannot distinguish between payments from patients and copay coupons, the coupons can be used to speed patients to their out-of-pocket maximum even when they have not paid the share their insurance plan requires.
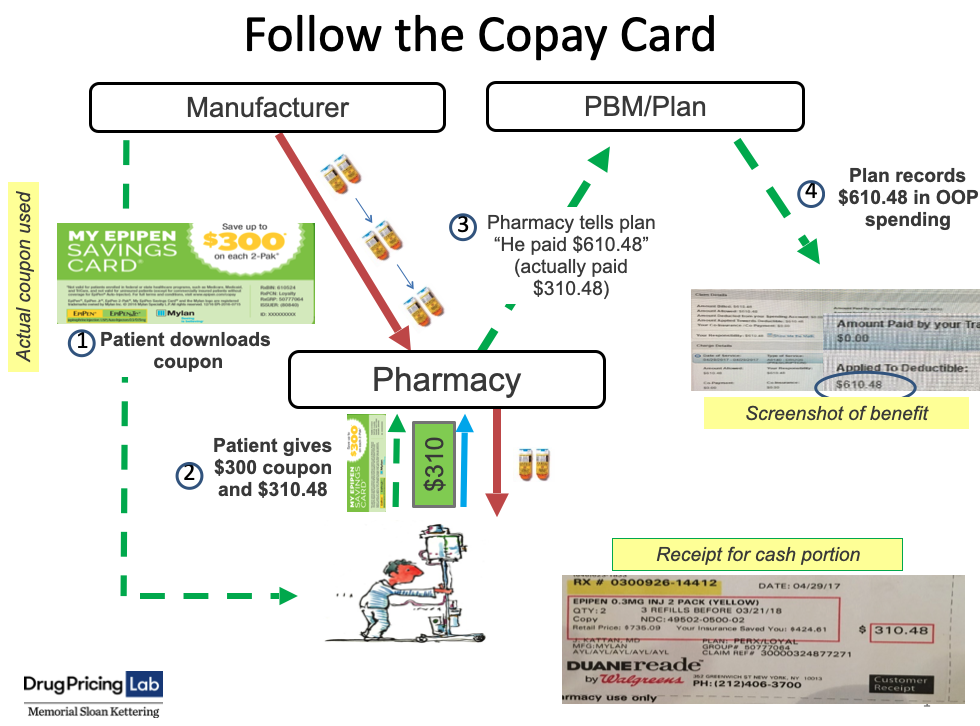
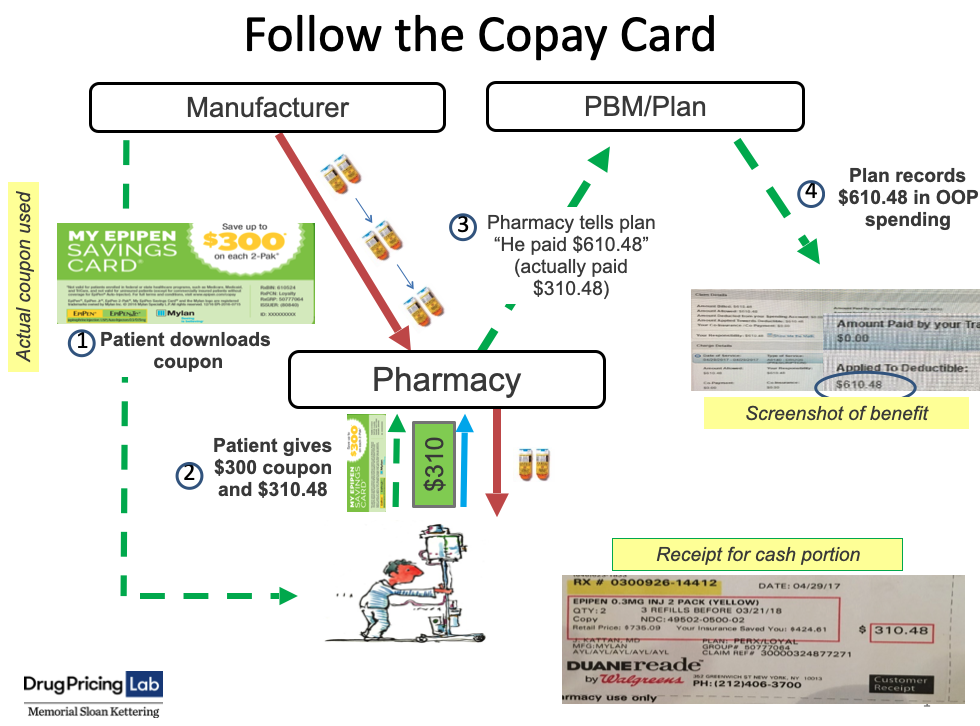
The transactions displayed in the image below (download full-size slide here) show a real-world interaction on April 29, 2017 between a patient, pharmacy, manufacturer, and insurer involving the use of a copay coupon. Mylan Pharmaceuticals offers a $300 coupon for patients to use to purchase a 2-pack of Epipens, which costs $610.48. When the patient arrived at the pharmacy to pick up the prescription, they presented the coupon and were asked to pay the remainder of the cost, $310.48. The pharmacy dispensed the drug for $310.48, but still reported to the patient's insurance plan that the customer had paid the full price of $610.48. The plan recorded this as the patient's expenditure and applied it to their deductible, even though the patient only covered half the cost. In this way, copay coupons allow patients to artificially accelerate through their out-of-pocket maximum, shifting the financial responsibility of drug costs to the insurer.